🌿 How to Know If Your Symptoms Are Part of Perimenopause — Or Something Else
If you’ve ever asked yourself:
“Is this perimenopause… or is something wrong with me?”
—you’re not alone.
One of the most confusing (and frustrating) parts of perimenopause is that its symptoms overlap with almost everything:
stress
burnout
thyroid issues
gut problems
anxiety
nutrient deficiencies
nervous system overload
And too often, women are told:
“It’s just stress.”
“Your labs are normal.”
“That’s just aging.”
But your body isn’t vague — it’s precise.
You just need the right language to understand it.
This article will help you:
Identify whether a symptom is likely perimenopause-related
Recognize signs of non-hormonal imbalance
Use Ayurveda and Traditional Chinese Medicine (TCM) as diagnostic lenses
Know who to turn to — and when
🌙What Perimenopause Actually Is (and Isn’t)
Perimenopause is the transition phase before menopause, often beginning between ages 35–50.
It’s marked by:
fluctuating estrogen and progesterone
increased nervous system sensitivity
changes in metabolism, digestion, and sleep
reduced resilience to stress
Importantly:
👉 Perimenopause amplifies existing imbalances rather than creating everything from scratch.
That’s why two women can have completely different experiences.
🔍 The Key Question to Ask (Before Googling Symptoms)
Instead of asking “What is wrong?”, ask:
Is this symptom cyclical, progressive, or situational?
This single distinction matters more than most lab tests.
Let’s break it down.
🌿 Signs Your Symptom Is Likely Part of Perimenopause
1. The Symptom Is Cyclical or Erratic
Common examples:
anxiety that spikes before your period
sleep disruption that comes and goes
bloating that changes week to week
mood swings without clear triggers
Ayurveda:
This reflects Vata aggravation — irregularity, movement, fluctuation.
TCM:
This often shows Liver Qi instability, where hormonal shifts disrupt smooth flow.
👉 If symptoms wax and wane, hormones are likely involved.
2. Stress Makes Everything Worse
If emotional stress immediately worsens:
hot flashes
palpitations
digestion
sleep
fatigue
this is a hallmark of perimenopause.
Ayurveda:
Hormonal transition weakens Ojas (vital reserve), reducing stress tolerance.
TCM:
Stress stagnates Liver Qi, which directly affects hormones, digestion, and sleep.
👉 Perimenopause lowers your buffer — it doesn’t mean you’re weak.
3. Your Old “Healthy Habits” Stop Working
Signs include:
fasting now causes anxiety
cold smoothies lead to bloating
intense workouts leave you exhausted
caffeine suddenly triggers palpitations
Ayurveda:
Digestive fire (Agni) becomes more sensitive.
TCM:
Spleen Qi weakens, reducing metabolic stability.
👉 This is one of the clearest perimenopause markers.
🚩 Signs Your Symptom May NOT Be Perimenopause Alone
Perimenopause does not explain everything.
Here’s how to tell.
4. The Symptom Is Constant and Progressive
If something is:
worsening steadily
present every single day
unrelated to cycle or stress
it deserves deeper investigation.
Examples:
persistent pain
unexplained weight loss
extreme fatigue that doesn’t fluctuate
numbness or neurological symptoms
👉 Perimenopause symptoms fluctuate.
Constant decline needs evaluation.
5. Digestive Symptoms That Ignore Hormonal Rhythm
Red flags:
severe constipation or diarrhea with no cycle pattern
food reactions that escalate rapidly
blood in stool
sudden intolerances after illness or antibiotics
Ayurveda:
This may indicate Ama accumulation beyond hormonal influence.
TCM:
Possible Damp-Heat or Gut Qi damage.
👉 These need gut-focused care, not just hormone talk.
6. Emotional Symptoms With No Physical Anchoring
If anxiety or low mood:
doesn’t change across the cycle
worsens in the morning consistently
feels disconnected from the body
this may point to:
nervous system burnout
trauma load
neurotransmitter imbalance
👉 Hormones interact with the nervous system — but they aren’t always the root.
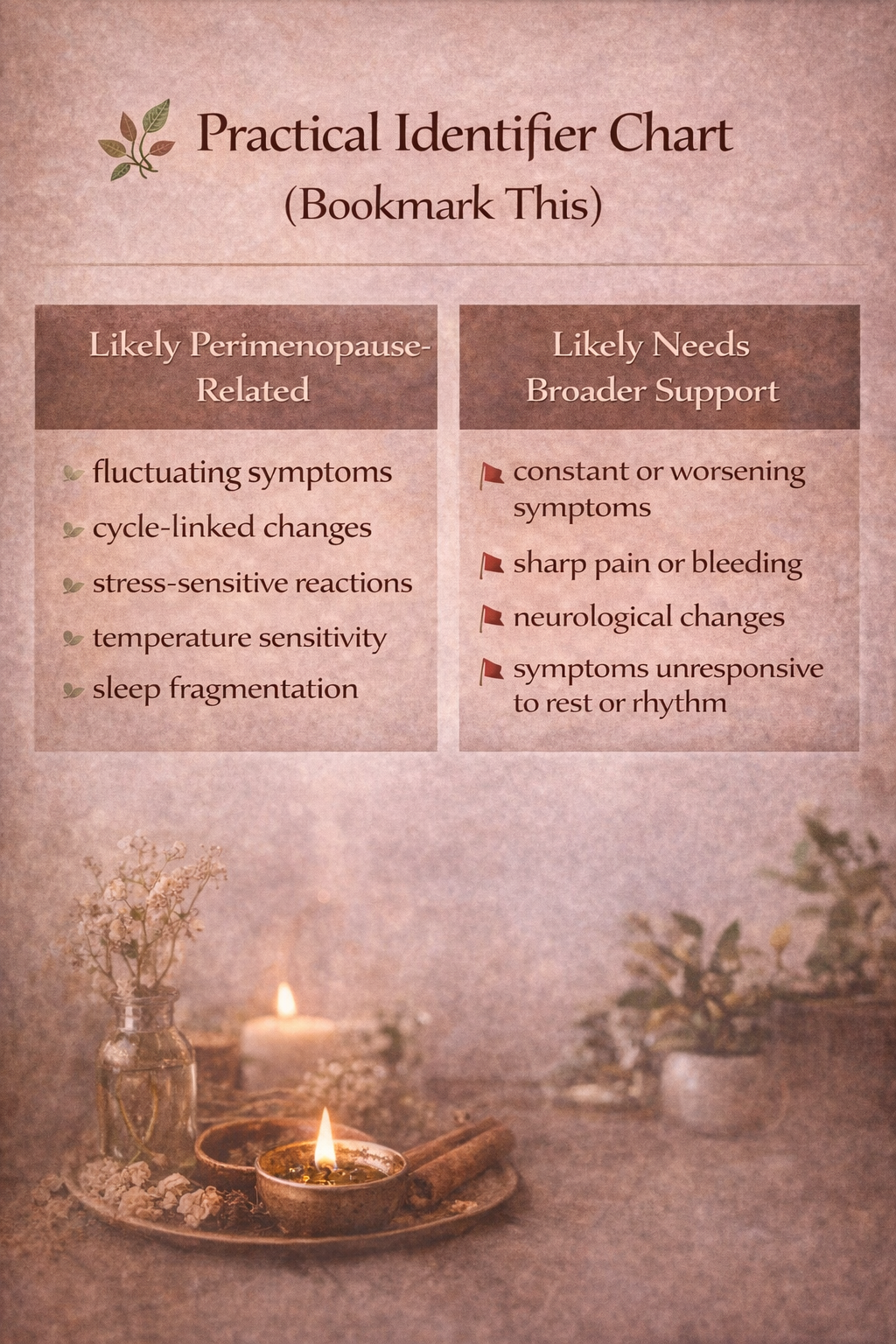
🌿 Practical Identifier Chart (Bookmark This)
Likely Perimenopause-Related
fluctuating symptoms
cycle-linked changes
stress-sensitive reactions
temperature sensitivity
sleep fragmentation
Likely Needs Broader Support
constant or worsening symptoms
sharp pain or bleeding
neurological changes
symptoms unresponsive to rest or rhythm
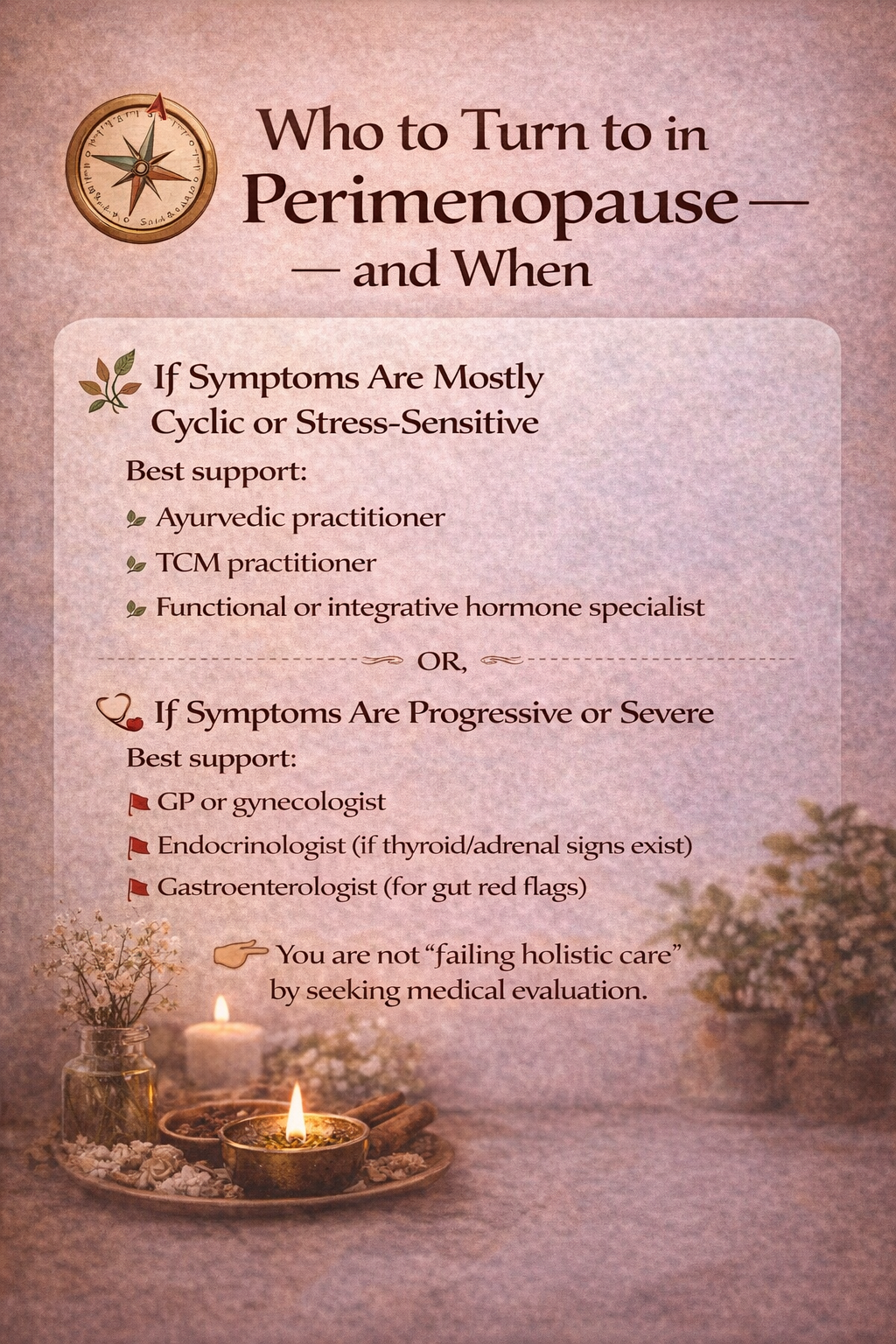
🧭 Who to Turn to — and When
This is where many women get stuck.
Here’s a grounded map.
🌿 If Symptoms Are Mostly Cyclical & Stress-Sensitive
Self-Regulate First (and How to Learn It)
If your symptoms fluctuate, intensify with stress, ease with rest, or feel unpredictable rather than steadily worsening, self-regulation is often the most appropriate first step.
The good news: self-regulation is not a talent or intuition you either have or don’t have — it’s a skill that can be learned.
In Ayurveda, this begins with understanding your dominant dosha — your body’s energetic pattern — and how it responds to stress, stimulation, food, temperature, and rhythm. When you understand whether your system is more Vata, Pitta, or Kapha-influenced, regulating your nervous system becomes far simpler and more precise. You can identify your dosha by (going through a short FREE Quiz)
From there, small practices — like warmth for Vata, cooling for Pitta, or gentle activation for Kapha — can quickly calm symptoms and restore internal balance. These are simple, body-based adjustments, not long protocols.
As the nervous system settles, the body communicates more clearly. Digestion improves, sleep stabilizes, and symptoms become easier to interpret — helping you recognize whether what you’re experiencing is part of perimenopause, cumulative stress, or something that truly needs additional medical or therapeutic support.
Self-regulation isn’t avoidance.
It’s learning your body’s language first — so you know exactly what kind of help to seek next.
Professional Support
If however you feel you prefer to consult a specialist, I recommend:
Best support:
Ayurvedic practitioner
TCM practitioner
Functional or integrative hormone specialist
Focus areas:
nervous system regulation
digestion and metabolism
lifestyle rhythm
constitution-based nutrition
🩺 If Symptoms Are Progressive or Severe
Best support:
GP or gynecologist
Endocrinologist (if thyroid/adrenal signs exist)
Gastroenterologist (for gut red flags)
👉 You are not “failing holistic care” by seeking medical evaluation.
🌿 Exceptions!
Hair Loss in Perimenopause
While many perimenopause symptoms tend to be cyclical or stress-sensitive, there is an important exception worth naming clearly: hair thinning or hair loss.
Hair loss can absolutely be part of perimenopause — even when it does not follow an obvious monthly or cyclical pattern.
This is because hair responds to longer-term hormonal, metabolic, and nervous system shifts, rather than short-term fluctuations.
Why Hair Loss Often Isn’t Cyclical
Hair grows in multi-month cycles, not daily or weekly ones.
So changes in hormones, stress, digestion, or nourishment may take months to show up as increased shedding or thinning.
In perimenopause, hair loss often reflects:
gradual progesterone decline
relative androgen dominance as estrogen falls
cumulative stress on the nervous system
reduced nourishment reaching peripheral tissues
This makes hair loss feel:
steady rather than fluctuating
slow to appear
slow to reverse
Even though it is still hormonally influenced.
2. SI Joint Pain and Structural Inflammation
Another symptom that may not follow a cyclical perimenopause pattern — yet is still commonly linked to this transition — is SI joint pain.
Once inflammation or instability develops in the sacroiliac joint, symptoms often become mechanical rather than cyclical. This means pain may worsen with certain movements, positions, or loading patterns, regardless of where you are in your cycle.
Why SI Joint Pain Behaves Differently
Perimenopause increases:
connective tissue vulnerability
joint laxity due to hormonal shifts
nervous system sensitivity
recovery time after strain
When these factors combine with past asymmetries, repetitive loading, or compensatory movement patterns, the SI joint can become irritated or unstable.
Once this happens:
pain may persist daily
symptoms may worsen with walking, standing, or rolling in bed
rest alone often doesn’t resolve it
the pain no longer tracks with hormonal fluctuations
This doesn’t mean hormones are irrelevant — it means the issue has moved into the structural and neuromuscular layer.
A Note From Lived Experience
I have first-hand experience with chronic SI joint dysfunction, including how it can worsen with movement once inflammation and instability set in — and how confusing it can feel when pain no longer follows hormonal or cyclical patterns.
What ultimately helped was not waiting for hormones to “settle,” but addressing the issue at its structural and neuromuscular root through specific, corrective movement and nervous system support.
If SI joint pain is part of your experience, I’ve written a dedicated article that goes much deeper into:
why SI joint pain shows up in perimenopause
what actually makes it worse
and how to begin restoring stability safely
👉 Read: How to Heal Si-Joint Pain in Perimenopause and Stop The Flare-up Cycle
🌸 The Ayurvedic + TCM Truth About Perimenopause
Both systems agree on one thing:
Perimenopause is not a disease. It is a reorganization of energy.
Ayurveda sees it as a Vata-dominant transition. TCM sees it as a shift in Kidney and Liver dynamics.
Symptoms arise when the system lacks:
warmth
rhythm
grounding
safety
Not when you “fail at health.”
🌙 Take This With You
Your symptoms are not random.
They are signals asking for interpretation, not suppression.
When you learn to ask:
“Is this hormonal, nervous, digestive — or cumulative?” your body becomes easier to understand.
And when you understand your body, you stop fighting it — and start working with it.
💌 Want Support Navigating This?
If you’re unsure whether your symptoms are perimenopause-related or something else, gentle nervous system regulation is often the safest first step.
That’s why I created the PeriPower Nervous System Reset — a short, hands on body-based guide to help your system settle, soften, and feel safe again. When the nervous system calms, symptoms become easier to read, digestion improves, and your body can clearly signal what kind of support it truly needs.
Here are a few more posts you may enjoy: